Chronic pain is a complex condition that affects millions of people worldwide. It can have a significant impact on an individual’s quality of life, making everyday activities challenging and limiting their overall functionality. In order to effectively manage chronic pain, it is essential to have a comprehensive understanding of its causes, symptoms, and treatment options. This article delves into the topic of chronic pain, with a particular focus on Chronic Pain ICD 10, a coding system used to classify and document different types of chronic pain.
Chronic pain refers to persistent or recurrent pain that lasts for an extended period of time, typically exceeding three months. Unlike acute pain, which serves as a warning sign of injury or illness, chronic pain persists long after the initial injury or condition has healed. It can be caused by various factors, such as injury, nerve damage, inflammation, or underlying medical conditions. The physical sensations associated with chronic pain can range from mild discomfort to debilitating agony, significantly impacting an individual’s physical and mental well-being.
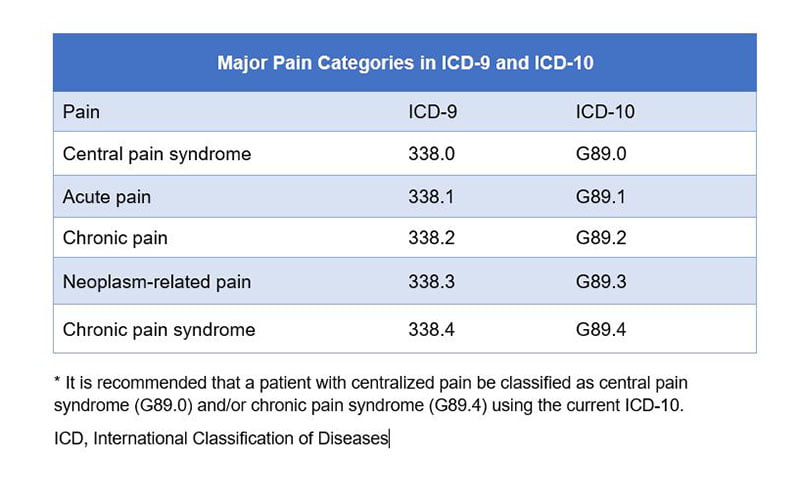
ICD 10, which stands for International Classification of Diseases, 10th Revision, is a globally recognized coding system used by healthcare professionals to classify and document diseases, disorders, and conditions. Chronic Pain ICD 10 provides a standardized way to categorize and describe different types of chronic pain. This coding system plays a crucial role in medical billing, research, and healthcare management.
Accurate and detailed coding of chronic pain using ICD 10 is essential for several reasons:
Chronic pain can stem from various underlying causes. Some of the most common factors contributing to chronic pain include:
Accurate diagnosis of chronic pain is crucial for effective management. Healthcare professionals employ various methods to diagnose chronic pain, including:
Managing chronic pain often involves a multimodal approach, tailored to the individual’s specific needs. The following are common treatment options used to alleviate chronic pain:
A: The ICD 10 code for chronic pain depends on the underlying cause or condition. Codes from the M79 category, such as M79.1 (Myalgia), M79.2 (Neuralgia and Neuritis), or M79.7 (Fibromyalgia), are commonly used to classify chronic pain.
A: Chronic pain can significantly impact an individual’s ability to perform daily activities and engage in employment. In some cases, chronic pain may meet the criteria for disability as defined by the Social Security Administration (SSA).
A: While there is no definitive cure for chronic pain, it can be effectively managed through various treatment modalities. The goal of treatment is to improve the individual’s quality of life, reduce pain intensity, and enhance functionality.
A: Chronic pain can lead to emotional distress, anxiety, depression, and reduced overall quality of life. The persistent nature of chronic pain can have a profound impact on an individual’s mental well-being, often requiring psychological support alongside physical treatments.
A: Adopting certain lifestyle modifications can complement medical treatments and improve chronic pain management. These may include regular exercise, stress reduction techniques, maintaining a healthy diet, getting adequate sleep, and avoiding smoking or excessive alcohol consumption.
A: Yes, there are numerous support groups and organizations dedicated to providing resources, education, and support for individuals living with chronic pain. These groups offer a platform for sharing experiences, coping strategies, and connecting with others facing similar challenges.
Chronic pain is a complex and challenging condition that affects millions of people worldwide. Understanding Chronic Pain ICD 10 and its coding system is essential for accurate documentation, research, and effective management of chronic pain cases. By diagnosing the underlying causes and implementing comprehensive treatment plans, healthcare professionals can help individuals living with chronic pain find relief, improve their quality of life, and regain functionality.
Recommended other topics: Obesity ICD 10-Understanding and Managing Obesity









© InfoDoot. All Rights Reserved.